A ganglion cyst is a very common bump in the hand and wrist. This type of cyst comes from a joint or tendon in the hand and wrist. The most common location is the back of the wrist (see image below). A ganglion cyst can occur in people of all ages. The cause of a ganglion cyst is unknown in most cases. One theory is that the cyst arises from joint fluid which has leaked from a small opening in the joint. The cyst is filled with a thick, jelly-like fluid and usually has a connection with a joint or tendon below.
What are the symptoms? Many people notice that the cyst fluctuates in size. In some cases the cyst can go away on its own. In many cases the cyst is not painful but in other cases, the cyst can cause pain and limited range of motion. Now you know what a ganglion cyst is. What is the best ganglion cyst treatment? Please read on.

Most ganglion cysts are diagnosed by history and physical exam by a trained physician. Since ganglion cysts are fluid-filled, a light shined directly on the mass will light up the cyst. X-ray, ultrasound, and MRI testing are not usually required to make the diagnosis in typical cases. Hand surgeons are experts in diagnosis of ganglion cysts in the hand and wrist.
What are the treatments available? There are three common ganglion cyst treatment options:
OBSERVATION: Also known as watch and wait. Since ganglion cysts are benign (not cancer), surgery is not required to remove them. Cysts which are not painful and do not interfere with function can be left alone and monitored. Some cysts can go away on their own. If the cyst becomes larger, painful, or interferes with function, further options should be discussed.
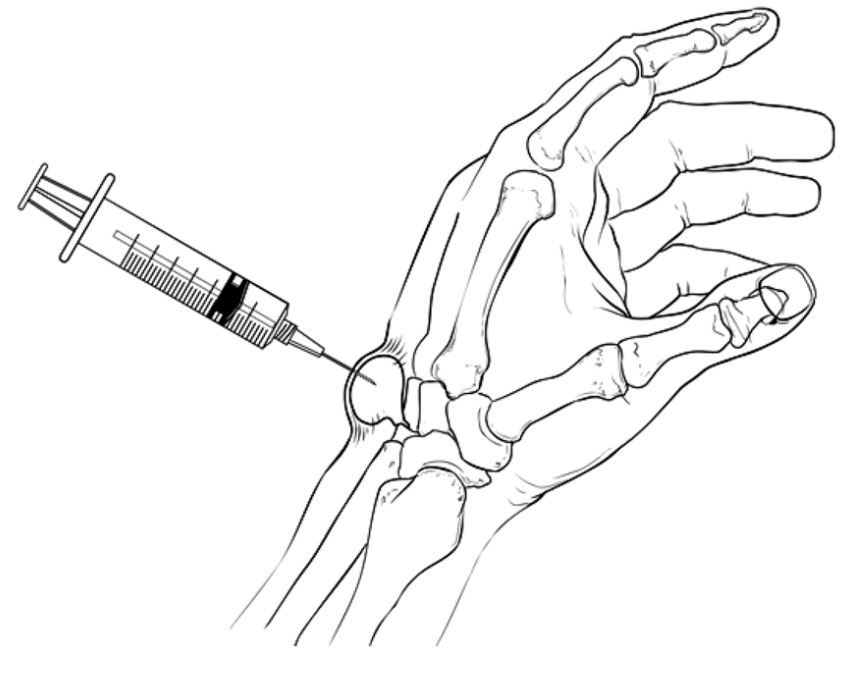
ASPIRATION: Also known as drainage with a needle. The cyst can be punctured and the thick fluid removed using a needle under sterile conditions. This is a quick procedure which is performed in the office. There is a high chance that the cyst comes back, however. There is a small risk of bleeding, pain, and infection from this procedure. Do NOT try this at home!
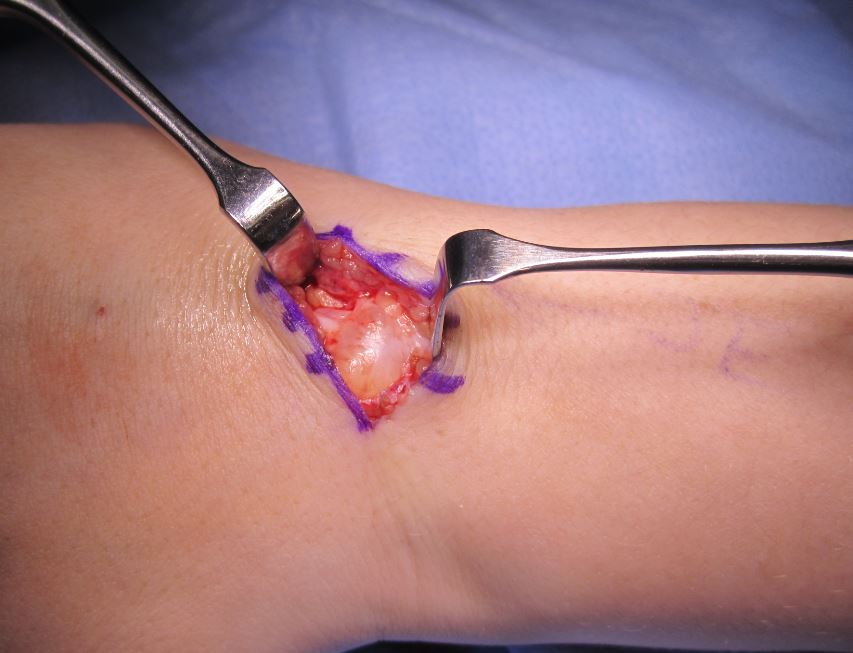
SURGICAL EXCISION: Finally, surgery is ganglion cyst treatment option. This surgery requires an incision and it is performed in the operating room. During surgery, the cyst is removed including the base which goes down to the joint. Removing the connection to the joint reduces the chance of cyst recurrence. Gardeners realize that the roots of the weed need to be removed, or else it will grow back.
In the past, some physicians have recommended simply popping the cysts by hitting them with a heavy book or Bible. For this reason ganglion cysts have been called “Bible cysts.” This is not recommended since damage can be done to the surrounding area, and most cysts recur with this technique.
What is the recovery from ganglion cyst excision surgery? Ganglion cyst excision is performed on an outpatient basis. Most people can return to light duty work in a few days as the pain and swelling subside. Hand therapy is sometimes helpful after this procedure to improve range of motion and strength. Patients should avoid forceful use of the hand for approximately 4 weeks after surgery. Normal use of the hand is resumed as comfort allows. Complications from surgery include cyst recurrence (5-10%), wrist stiffness, scar tissue, and infection.
The ganglion cyst images are copyright Dr John Erickson and the cyst aspiration drawing is copyright AAOS OrthoInfo. The video is courtesy of American Society for Surgery of the Hand.











